ADA - Americans With Disabilities Act
Bentek - Online Benefit Enrollment
Disability Insurance - Short Term and Long Term
Discounts for Employees-Wellness
Employee Assistance Program (EAP)
Employee Benefits Highlight Guide and Rates
Employees Leaving the District
Flexible Spending Account (FSA)
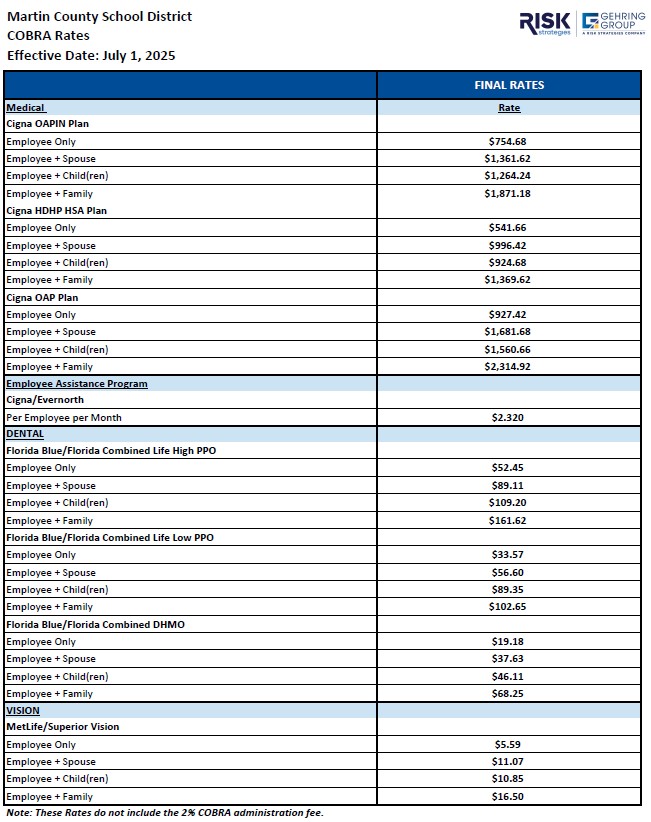
COBRA
What is COBRA coverage?
COBRA coverage is a continuation of Plan coverage required under Federal law.
COBRA coverage allows same coverage, in the same Plan, where employees/retirees and other eligible participants/dependents are losing eligibility of coverage. Each qualified beneficiary who elects COBRA will have the same rights under the Plan as other participants or beneficiaries covered under the component or components of the Plan elected by the qualified beneficiary, including open enrollment and special enrollment rights.
COBRA (and the description of COBRA coverage contained in this notice) applies only to the group health benefits offered under the Plan (the Medical, Dental, Vision, EAP and Health FSA components, as applicable) and not to any other benefits offered under the Plan or by Plan Sponsor.
Employment Termination
If an employee separates employment from MCSD, insurance will continue through the end of month in which separation occurred. COBRA continuation of coverage may be available as applicable by law. Cobra-eligible employees will receive a Cobra information packet from WEX, the District's third-party administrator. Those who wish to continue their coverage under Cobra must work directly with WEX regarding eligibility, enrollment and payment. WEX can be reached by phone at 866.451.3399 or online at www.wexinc.com.